Despite the availability of free cervical cancer screening in Nairobi, a recent study reveals that fewer than half—45.3%—of sex workers have been screened in the past year.


Researchers identify a combination of factors preventing access, including fear of a positive diagnosis, inconvenient clinic hours, misinformation, and cultural stigma about the screening process.
Cervical cancer, if detected early, is highly treatable. Yet many sex workers, particularly those living with HIV, are at a higher risk due to HPV infection, which can lead rapidly to cervical cancer. Studies show that many sex workers lack awareness of the link between HPV and cervical cancer, compounding the risks. A recent survey published in Therapeutic Advances in Infectious Disease found that 77.6% of respondents cited inconvenient clinic hours, and nearly 40% mentioned that stigma linked to cultural beliefs and misconceptions about cervical cancer further dissuaded them from getting screened.
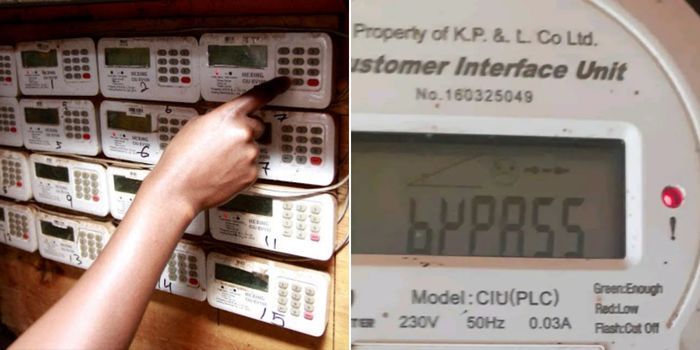
The study, conducted between August 2022 and January 2023 among female sex workers living with HIV in Nairobi, also highlighted logistical issues. Over a third of participants lived more than 10 kilometers from the nearest clinic, making transportation costs and time commitment significant obstacles. One respondent shared that many sex workers, who often work at night and sleep during the day, found clinic hours from 8 a.m. to 5 p.m. inaccessible.
Misunderstandings about the screening process further deterred participants. Two-thirds of respondents expressed discomfort with the procedure, fearing pain or negative results. Cultural beliefs also contributed to hesitancy, with some participants believing cervical cancer results from promiscuity or witchcraft, further fueled by the societal stigma against both sex work and HIV.
The Swop health facilities network, which offers free sexual health services to Nairobi’s sex workers, has provided free cervical cancer screenings, but uptake remains low. Data from 2019 showed that only 5% of HIV-positive sex workers were screened for cervical cancer that year, mirroring trends across other regions of Kenya.
To address these barriers, researchers recommend several strategies, including extending clinic hours, offering mobile screening units, and implementing community-based education to address myths and reduce stigma. Additionally, training healthcare workers in culturally sensitive care could bridge the gap between service availability and uptake. As cervical cancer remains the second most common cancer among Kenyan women, these measures could significantly improve screening rates and reduce preventable deaths in this high-risk population.