Kenya’s ambitious Social Health Authority (SHA) initiative has come under heavy criticism following an alarming report by Auditor General Nancy Gathungu. The report reveals that despite investing Ksh.104.8 billion in the SHA system, the government neither owns nor controls the infrastructure or intellectual property rights associated with it. This revelation has sparked widespread concern about the project’s transparency, financial viability, and long-term impact on healthcare access for citizens.


Ownership Concerns and Government Oversight
According to the Auditor General, the system’s ownership remains with the private consortium that developed it, effectively stripping the government of authority over the platform.
“The ownership of the system, system components, and all intellectual property rights shall remain in the ownership of the consortium,” Gathungu stated.
This arrangement means that SHA contributions and claims made by health facilities will continue to fund a system over which the government has no control. The Auditor General warned that this creates a significant risk for public funds and could undermine the delivery of healthcare services.
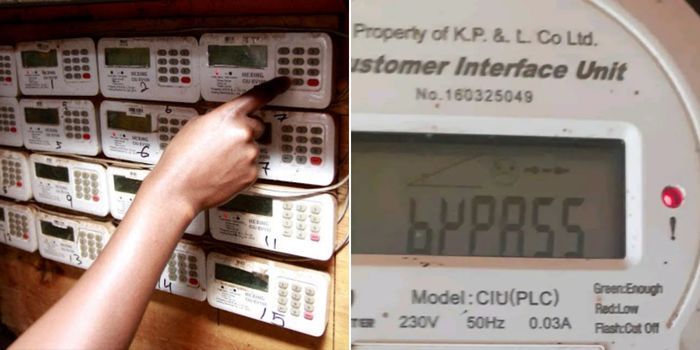
Procurement Irregularities and Legal Violations
Adding to the controversy, the procurement process bypassed competitive bidding. Instead, the contractor was sourced through a Specially Permitted Procurement Procedure, a move that violates Article 227(1) of the Kenya Constitution 2010.
“This process was contrary to Article 227(1) of the Constitution, which requires fair, equitable, transparent, competitive, and cost-effective procurement,” the report noted.
The project also circumvented the procurement plan and medium-term expenditure framework, violating Section 53(7) of the Public Procurement and Asset Disposal Act, 2015.
Financial Viability and Citizen Impact
The financing model projects Ksh.111 billion in revenue over a decade, sourced from SHA member contributions, health facility claims, and track-and-trace solution charges. However, the lack of a baseline survey raises concerns about its feasibility and potential to increase healthcare costs for citizens.
“The projected revenues include 5% deductions from claims made by health facilities, effectively increasing healthcare costs for citizens by the same margin,” Gathungu highlighted.
Additionally, revenues must be transferred to an escrow account daily or weekly, but the contract does not disclose the signatories to this account, raising further transparency issues.
Contract Restrictions and Legal Ramifications
The SHA contract prohibits the government from developing a competing system, limiting its ability to adapt to technological changes or growing needs.
“The government is barred from accessing the system to build a competing product or service,” Gathungu stated, cautioning that this provision could cripple future innovation.
Furthermore, any disputes related to the project will be resolved by the London Court of International Arbitration, sidelining local legal mechanisms and raising sovereignty concerns.
Broader Management Failures
The Auditor General’s report also highlighted systemic management flaws, including noncompliance with employment laws and insufficient staffing for people with disabilities.
“Three hundred and eighty-six employees earned a net salary below one-third of their basic salary, contrary to Section 19(3) of the Employment Act, 2007,” Gathungu revealed.
Moreover, only 2.3% of SHA staff are people with disabilities, far below the 5% mandated by public service policies.
Conclusion
The Auditor General’s findings underscore serious flaws in the SHA project’s procurement, management, and operational framework. The lack of government ownership, financial oversight, and transparency could jeopardize Kenya’s healthcare future, with citizens ultimately bearing the brunt of increased costs and inefficiencies.